How could patients better
better access Doctors in BC?
- Service Design Jam
Overview
In 2023 I worked with a design mentor on a Service Design Jam. I gave myself the challenge of completing a full design cycle in 1 week, from scoping to a completed service blueprint. The result demonstrates how I go about design thinking under pressure.
Sectors
Medical services, Healthcare, Medical technology
Team
Just me
Methods & Tools
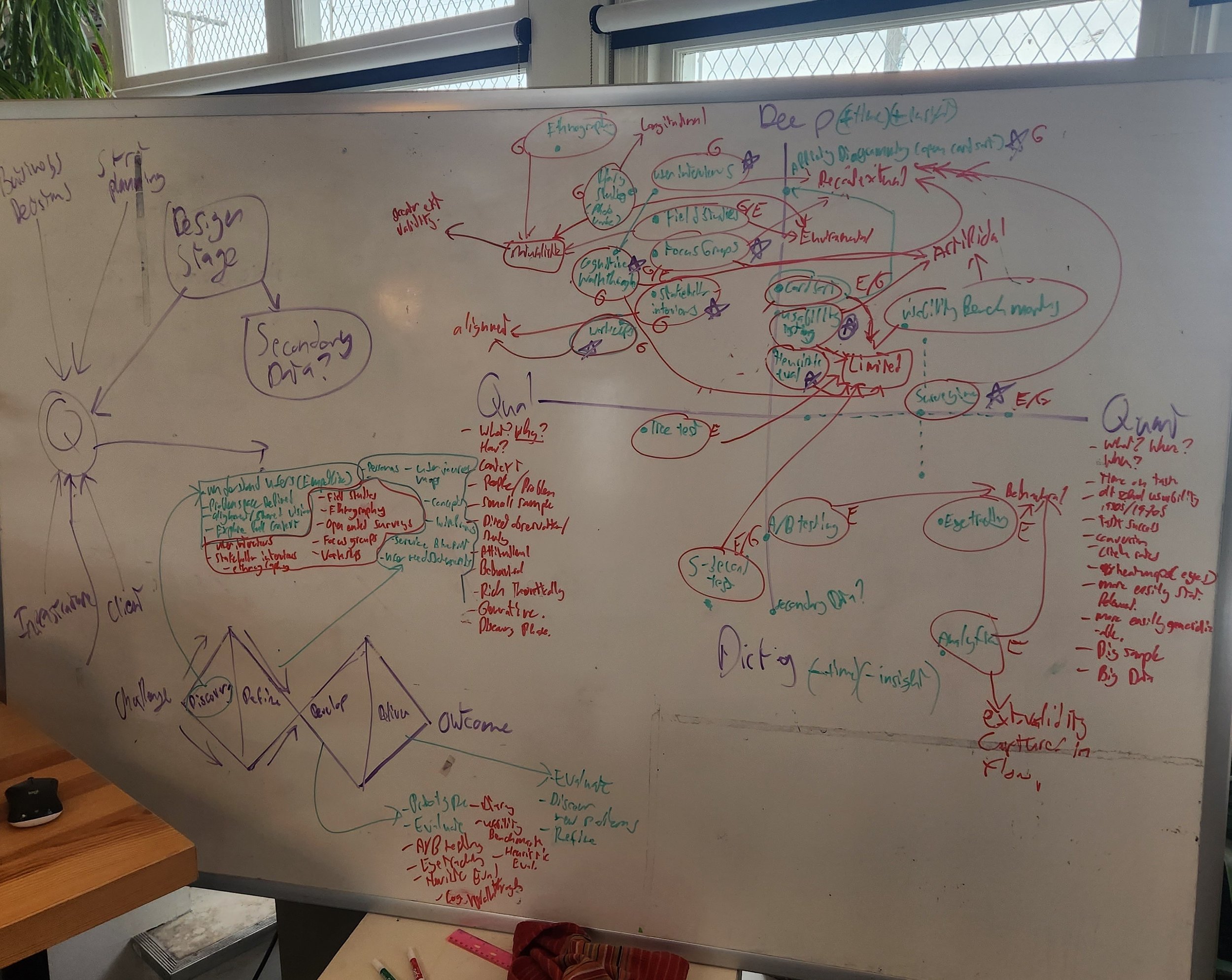
Structured interviews, Secondary data, Affinity diagramming, Service blueprinting, White boarding, Miro
Deliverables
Presentation, User need statements, Service blueprint
Background
In 2023 it seemed like I was hearing from everyone I knew who had been to the hospital, or worked in one, how the medical system in BC was facing massive problems in the aftermath of the COVID pandemic. Patients were waiting up to 10 hours or more, and generally not seeking care for issues that would then snowball and become more acute. My nurse friends were burning out, and my doctor friends couldn’t see an end in sight. This was accompanied by a seemingly endless number of reports, stories, and recommendations about how to improve our public healthcare system. This seemed like this definition of a wicked problem.
Defining the Problem Space
At the time I was working with a design mentor, and brought up these issues. They came up with the idea of a design jam, restricted to one week, where I would go from ideation to prototype with a solution to address healthcare system problems from the prospective of a client. I was asked to take the following prompt, with no other context, and come back in a week with a deliverable:
“HealthLabs is a large health tech organization looking to connect patients to doctors in their area better. They hired you as a Service Designer to work with the HealthLabs service design team to determine how patients could better access doctors and create a service blueprint outlining this experience.”
I started by breaking down the question into it’s component parts. I asked:
Who are the users I am designing for? (Orange)
What constraints do I have to work with? (Red)
What am I designing for? What metrics are guiding this design (Light blue)
HealthLabs is a large health tech organization looking to connect patients to doctors in their area better. They hired you as a Service Designer to work with the HealthLabs service design team to determine how patients could better access doctors and create a service blueprint outlining this experience
Based on this, I decided that there were two user groups in this challenge, both patients and doctors. Therefore experiences for both user groups would need to be considered in this service. The constraints were that I needed to connect patients in their area, which I further defined as “in Vancouver, BC”. Finally, the only measurable term in the prompt was “better” which I took to mean “more” and “better quality than the current base line of care”. With these in mind I formulated some initial research questions, to better understand the context of the problem space. They were:
RQ1: How do patients currently access care from doctors in Vancouver?
RQ2: What are the key limitations to patients in accessing care from doctors in Vancouver?
RQ3: What are the key limitations to doctors in providing care for patients in Vancouver?
RQ4: What would patients and doctors hope to see change in how patients access care in Vancouver?
With these questions, and the clock ticking, I developed a design research plan to answer each of these questions with appropriate methods, and further understand both needs and pain points of each user group. All of which quickly ran into constraints.
Design Research
My ideal methodology for learning more about the healthcare system in BC looked something like this:
I planned to start with stakeholder interviewing with nurses to better understand how the medical system in Vancouver works. I would then use my personal connections to doctors in the medical system in Vancouver, as well as to fellow patients like myself, to conduct a series of semi-structured user interviews to understand barriers, needs, and pain points. These would be followed up with short surveys to better understand the quality of care that patients were currently experiencing, and the ways that care had changed since the COVID pandemic for doctors.
However, it just so happened that none of my connections in the medical system were available for interviews or surveys within the week I was working. My whole research plan wouldn’t work. So I decided to pivot, and came up with a new plan which when completed, looked like this:
I began by reviewing secondary data. This included grey literature, reporting, position papers, and other sources that gave an explanation of how the medical system in Vancouver worked at a systems level. I was also able to conduct one user interview with a doctor, and five interviews with patients. Patients talked about habit change, how since COVID they had become much more comfortable with using Telehealth services to access a walk-in doctor. The most common through line in the patient interviews was the lack of, and need for family doctors, and how the model of community care through local family doctors had both immediate and systemic effects on health outcomes as a whole for people in Vancouver. This led to difficulty following up on requisitions, problems where patients left treatment until a problem became acute, or where proactive care would have lessened the severity of painful symptoms. Speaking with a doctor about her practice, she spoke emphatically about burnout, and how not only was there a lack of physicians within the system in BC at large, but that those within the system were being stretched to the breaking point and leaving the public care system for private clinics, or other provinces.
All of these findings were included in an open ended thematic analysis, Which I used to synthesize user need statements:
Reyaz needs consistency in how he receives healthcare do that he can make informed choices about his health without having to keep track of all his tests, diagnoses, and prescriptions.
David is aging and needs a family doctor in order to proactively take care of his health.
Erika wants the convenience of using a telehealth provider, with the personalized knowledge of the family doctor she used to have, in order to manage her chronic health conditions
Imogen is a doctor who needs help alleviating the backlog of patient care after the COVID-19 Pandemic in order to avoid burnout.
With these user need statements in mind, I started iterating ideas for a service that could address these important, and deeply interconnected problems, while taking advantage of the opportunities for behaviour shift in the aftermath of the Pandemic.
Iteration and Blueprint
When whiteboarding, I tend to completely work through a whole idea before moving into another iteration. Over the course of a day, I worked through many different options and ideas for a completed service. I wanted to take a growth mindset approach with the theme of “behaviour change initiated by the COVID-19 pandemic”, and explore how these positive habit could be used as a foundation for a holistic service. I was also interested in finding a way for users to access not just doctors, but family doctors, as the interviews, secondary data and background reading I had conducted spoke extensively to both the lack of family doctors and the long term healthcare benefits to both individuals and the healthcare system of having more frequent and regular care.
With this in mind I developed an idea of a telehealth service called HealthLabs Connect. The system would work like other telehealth systems with three important differences. Firstly, the system would prompted patients for follow up care to develop a relationship with walk-in doctors. Over time, doctors would have the ability to choose new patients for their family care practice. Second, patients would be added to a list of potential family care patients for doctors. Third, all of this would be back-ended by a recent development of a patient centred data-system, CST Cerner, which enables physicians to access patient records across all instances of care while preserving privacy. The service allows doctors to find new patients, and enable community care physicians to help lessen the load on the healthcare system overall. Once doctors take on patients as their family doctor, patients still can access their family doctor via telehealth through HealthLabs Connect any time, in addition to in person visits as needed.
Click here to view the Service Blueprint
Reflections
I presented this project to my mentor for feedback. However, looking back on this project I think there are few areas I would improve upon:
Firstly, I gave limited space for understanding the incentive structure for doctors as a user group. While patients have very clear needs (and indeed, I can better emphatize with those needs) I feel that the lack of incentives in this system shows when you consider how doctors would be recruited for this service. Are there additional fees they can charge? Is it targeting newer doctors going into community care? These questions were unclear and an area for further exploration. I think this likely was a strcutural issue with my design research, and might have been better aligned if I had more access to doctors for interviews.
Secondly, I think another area for improvement is understanding differentiation for HealthLabs connect relative to other walk-in doctor telehealth services. The general premise was that this healthcare service would be the only one where eventually you stop needing a walk in doctor (like the marketing for the dating app Hinge: “the dating app designed to be deleted”). However, it isn’t clear that this is a strong enough differentiator, as walk-in doctors can and do take on patients in a family doctor capacity (though with an unclear frequency.) This is another area for exploration.